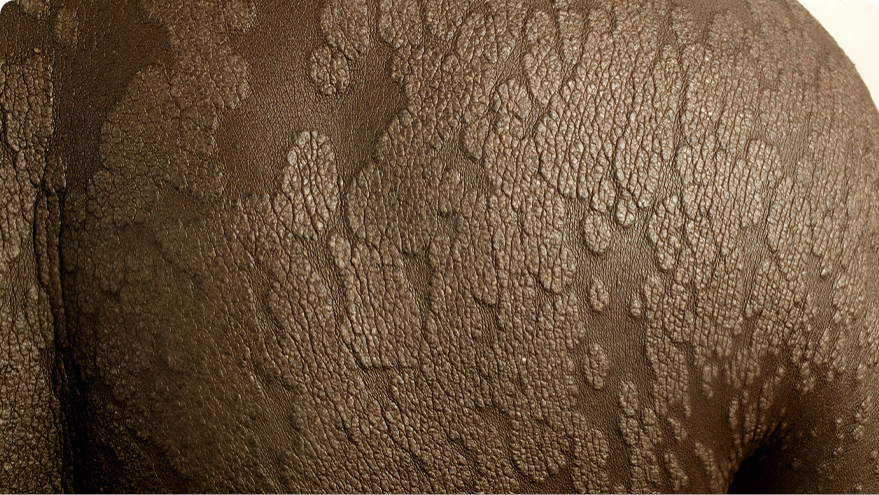
Psoriatic Arthritis
How can psoriasis, a disease that affects your skin, be associated with joint pain in psoriatic arthritis, too? Psoriasis and psoriatic arthritis are both believed to start with excess inflammation inside the body.
In fact, 1 out of 3 people with psoriasis will also experience joint symptoms, which is referred to as psoriatic arthritis. Since they can occur together, inflammation is believed to be a common source. However, one condition does not necessarily cause the other—either psoriasis or psoriatic arthritis can present itself first. Also, the severity of one does not determine the severity of the other. This means you can have severe psoriasis, but moderate psoriatic arthritis, or vice versa.



It is important to talk to your dermatologist or rheumatologist about any symptoms you are experiencing so they can appropriately manage your care.
Common psoriatic arthritis (PsA) symptoms include:



Swollen fingers and toes

Tender, painful, or swollen joints

Reduced range of motion of joints

Morning stiffness

Lower back, upper back, or neck pain

General fatigue

Change in nails,
such as pitting
or separation
from nail bed
If you are experiencing any symptoms of psoriatic arthritis listed above, it's important to tell your dermatologist or rheumatologist.
Getting Tested for Psoriatic Arthritis (PsA)
Although there are no definitive tests for PsA, your dermatologist or rheumatologist can make a diagnosis based on your medical history and a physical exam, along with other factors, such as:
- signs and symptoms (observed or patient-reported)
- multiple screenings
- laboratory test to help rule out other conditions
If you have any of the psoriatic arthritis (PsA) symptoms listed above, it’s important to tell your dermatologist or rheumatologist right away.
Treating PsA
Psoriatic arthritis is a chronic disease that should be treated in a timely manner. There are multiple treatment options for PsA that can help with joint symptoms and lessen your pain. PsA presents differently for everyone, so it’s important to connect with your dermatologist or rheumatologist to come up with a treatment plan specific to you.